Most people picture hypothermia as a dramatic outdoor emergency. We picture someone lost in a blizzard or stranded on the highway. But in the New York and New Jersey area, a more common setup is quieter: a power outage during a cold snap, an older building that can’t retain heat, or a space heater used unsafely. Add a baby who can’t explain what they’re feeling, or an older adult who may not notice the room getting colder, and the risk becomes very real.
Here’s the key point up front: ongoing exposure to cold temperatures indoors can cause hypothermia, especially in older adults and babies.
Let’s focus on facts, practical warning signs, and what to do during outages, so you can protect the people most vulnerable to indoor cold exposure.
Hypothermia: Symptoms & Overview
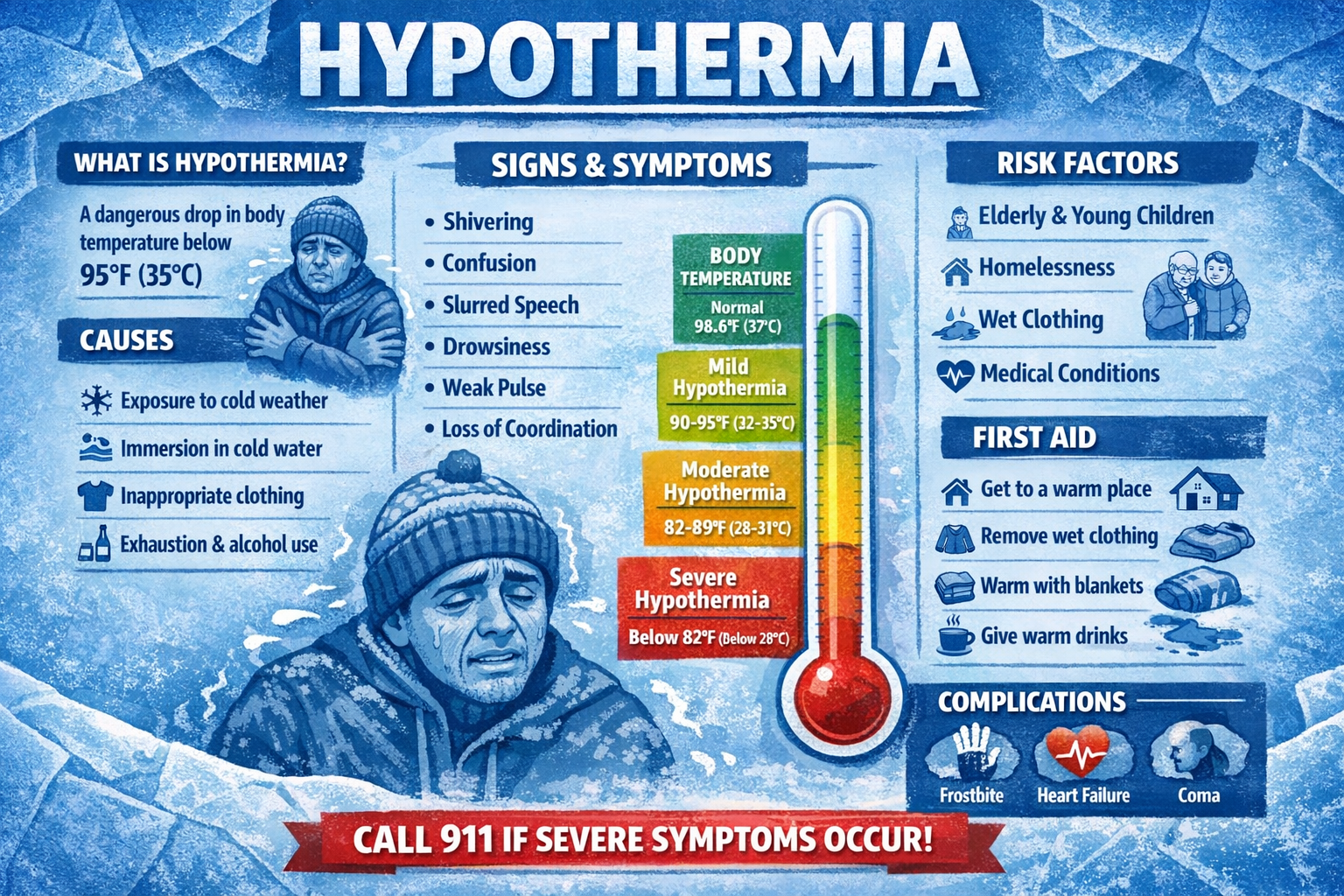
Hypothermia is abnormally low body temperature, generally defined as one’s core temperature drops below 95°F (35°C).
It’s considered a medical emergency because, as body temperature drops, the brain and body can’t function normally. Symptoms of hypothermia can start subtly and worsen over time. Generally, the symptoms are as follows:
- shivering (though shivering may stop as the temperature drops)
- slurred speech or mumbling
- slow, shallow breathing
- weak pulse
- clumsiness, confusion, or unusual sleepiness
Mild Hypothermia
Mild hypothermia is often the early stages of cold exposure, when the body is still fighting to hold onto core body temperature by generating more body heat. This is typically when someone feels cold and starts shivering, one of the body’s fastest ways to produce heat.
Signs of hypothermia in this stage can look “mild” at first, which is why indoor hypothermia can be missed, especially if a person is tired, bundled in blankets, or asleep. You might notice persistent shivering, cold hands/feet, pale or cold skin, or someone seeming unusually quiet and sluggish.
Even when symptoms seem mild, hypothermia can worsen if the indoor environment stays cold (no heat, drafts, damp clothing).
Moderate hypothermia
Moderate hypothermia is where the situation becomes much more serious because the body starts losing the battle to maintain core body temperature. As temperature drops, blood flow is redirected toward vital organs (a protective response), which can leave the skin and extremities even colder and make the person look pale, stiff, or “out of it.”
A key shift in moderate hypothermia is that shivering may slow down or even stop. Confusion becomes more noticeable, and the person may slur words, stumble, or seem disoriented—sometimes without realizing anything is wrong. These changes occur because cooling affects the brain and muscles, impairing judgment.
This is also the stage where some people experience a “cold shock” type response, such as rapid breathing, a racing heartbeat, or panicky discomfort, especially if they’ve had sudden exposure to cold air after sweating, bathing, or being in wet clothing. The bigger concern, though, is that the person’s temperature can become dangerously low and continue to fall.
Moderate hypothermia requires immediate medical care. If you suspect moderate hypothermia, especially if the person is confused, unusually sleepy, not shivering, or getting worse, call 911 or go to the nearest emergency room.
Severe hypothermia
Severe hypothermia is a life-threatening emergency. At this point, the body’s core body temperature is so low that normal brain and heart function can be impaired. The person may stop shivering, appear extremely drowsy, lose consciousness, or seem unresponsive. Breathing can become slow and shallow, and the pulse may be weak.
Severe hypothermia is especially dangerous because the person may not look like they’re in distress—sometimes they can appear calm, confused, or “sleepy,” even though their condition is dangerously low and worsening. Skin may feel very cold, and because blood flow is prioritized to the body’s core, fingers and toes can become numb and stiff.
This is also where survival time can become a concern. The longer the body remains severely cold, the higher the risk of severe complications. The most important message for readers: do not wait for a “certain amount of time” to pass if someone is showing severe signs of hypothermia.
Severe hypothermia requires emergency medical care immediately. Call 911. While waiting for help, follow first-aid guidance: move the person to a warm, dry area, remove wet clothing, and warm them gradually with blankets. Avoid rough handling or aggressive rewarming.
Factors to Keep in Mind: Why Hypothermia Occurs
| Risk factor at home | Why it matters | What to do right now |
| No heat / very low thermostat | Prolonged cool temps can cause hypothermia, especially in babies/older adults | Add dry layers/blankets, keep people together, seek safe warming options |
| Damp clothes/hair | Moisture accelerates heat loss | Change into dry clothing, dry hair, replace wet socks |
| Limited mobility / living alone | Harder to add layers, move rooms, or call for help | Check-in plan with family/neighbors |
| Exhaustion/dehydration | Increases risk of hypothermia | Warm fluids if available (non-alcoholic), rest, monitor symptoms |
| Unsafe heat source during outage | Carbon monoxide and fire hazards | Follow CDC/EPA generator and CO guidance |
Keep in mind that both cool indoor temperatures and exhaustion/dehydration are risk factors.
How do you get hypothermia indoors?
While indoors, hypothermia usually happens through one of these pathways:
1) The indoor temperature stays too low for too long
If heat is lost faster than the body can generate it, body temperature drops—especially if someone is sleeping, not moving much, or has limited ability to add layers.
2) You get chilled + damp (even inside)
Wet hair after a bath, sweaty clothes, or damp socks from tracked-in slush can speed heat loss. In winter, “damp + still” is a common problem.
3) You can’t respond normally to the cold
Older adults may be less aware of temperature changes, and babies can’t communicate symptoms the same way adults do. The Mayo Clinic specifically flags older adults and babies as higher-risk for hypothermia from cool indoor temperatures.
4) You’re exhausted or dehydrated
Being exhausted or dehydrated can increase the risk of hypothermia, even indoors. Cleveland Clinic notes that indoor hypothermia can occur surprisingly fast under the wrong conditions—especially if the thermostat is set very low or there’s no heat—and warns that a person who falls and can’t get up can be at risk.
How long does it take to get hypothermia?
It varies. It can happen in as little as 10–15 minutes if conditions are cold enough. There isn’t a universal timer because it depends on:
- indoor temperature
- how dry/wet the person is
- how much the person is moving
- age, body size, and underlying health
- whether they’re exhausted or dehydrated
What you can say confidently is:
- Hypothermia can develop more quickly in babies and older adults.
- Prolonged exposure to a cool indoor environment can be enough.
- In extreme indoor cold (for example, a home without heat in winter), risk increases sharply.
Who is most at risk at home?
Babies and young children
Babies lose heat faster than adults and may not show obvious “adult-style” symptoms. Baby symptoms can include cold and bright red skin, as well as very low energy.
Older adults
Older adults have a higher chance of being affected by cold and may have a harder time noticing when their body is getting too cold.
People who live alone or have limited mobility
If someone can’t easily add layers, move to a warmer space, or call for help. Indoor cold becomes riskier, especially during outages.
Anyone without reliable heat during power outages
Power outages often lead people to use alternative heat sources that can create other serious dangers, especially carbon monoxide exposure.
Power outages: how to stay warm without creating a new hazard
When the power goes out during winter storms, people often improvise—and that’s where preventable tragedies happen.
Carbon monoxide risk is the big one
During outages, alternative fuel sources for heating/cooking can cause carbon monoxide (CO) to build up indoors and poison people because CO is odorless and colorless.
Do not use generators, grills, camp stoves, or gasoline-powered equipment inside a home, garage, or near windows/doors. CO can cause sudden illness and death.
The U.S. EPA also provides guidance on protecting indoor air quality and using CO detectors during outages.
Safer “stay warm” approach during an outage
Without getting overly technical, the goal is to reduce heat loss:
- Put on dry layers (including socks and a hat)
- Use blankets and keep people together for warmth
- Close off unused rooms to conserve heat
- Keep a flashlight handy (avoid candles if possible)
- Check on older neighbors or family members regularly
If you’re caring for a baby or older adult, be extra cautious: their bodies may cool faster, and symptoms may be harder to detect early.
What to do if someone might be getting hypothermia at home
Stick to established first-aid guidance to avoid further heat loss:
- Move the person to a warm, dry location in the house. Ideally, somewhere where a heater or heat lamp can be used to keep their body warm.
- Remove any wet clothing from their body. Wet clothes in the cold weather will only make the loss of body heat even worse.
- Run the person a hot bath. Keep the water temperature at ## until they feel warm to the touch. Afterwards, dress them in warm clothing. Add layers of dry clothes to help stabilize them.
- Warm gently (blankets, warm environment)
- Act quickly and call emergency services if hypothermia is suspected.
Avoid “DIY fixes” that can backfire. Follow recognized first-aid recommendations rather than guessing.
Prevent Hypothermia with +MEDRITE
If you’re concerned about cold exposure symptoms or unsure what the next step should be, visit a +MEDRITE Urgent Care Center near you. Select “Book Appointment” at the top of the facility page closest to you and follow the steps. Or, simply walk in! If symptoms are severe, worsening, or you suspect hypothermia, call 911 or go to the nearest emergency room.